The Basics
When it comes to EEOICPA health benefits, many beneficiaries get confused about the services the Department of Labor (DOL) will and won’t pay for. Let me try and clear up some of this confusion.
The medical benefits available to living workers are generally the same under both Part B and Part E of the program. However, the DOL will only pay for services prescribed by a treating physician. Furthermore, the treating physician must provide evidence that the prescribed service is for treatment of an approved illness.
If you’re confused I’ll break this down a little more later in this post. For now, here is a list of some the medical benefits available to former workers approved under EEOICPA.
Medical Benefits List
- Prescription Drugs
- Doctor Copays
- Medical Travel
- Oxygen Supplies
- Home Health Care
- Durable Medical Equipment
- Housing Modifications
- Vehicle Modifications
- Vehicle Purchase
- Hospice Care
- Organ & Stem Cell Transplant
- Nursing Home
- Assisted Living
- Extended Care Facilities
- Medical Alert Systems
- Health Facility & Spa Membership
- Chiropractic Services
- Illness Screening Service
- Home Exercise Equipment
- Psychiatric Treatment
Not sure if you’re eligible? Click here to learn more
Which Costs Are Actually Covered?
To understand which medical expenses are covered we need to understand the definition of an “Accepted” illness. An accepted illness is the condition you list on your EEOICPA claim. For example, if you’re filing a Part B claim for chronic beryllium disease, chronic beryllium disease would be your accepted illness.
Once the claim has been filed and approved by the Department of Labor, medical bills related to the condition will be reimbursable.
The DOL will ONLY pay for treatment directly related to an accepted illness.
For example, if you have been approved for pancreatic cancer under EEOICPA, any treatment related to pancreatic cancer can be billed to the Department of Labor by the medical provider.
However, let’s say you also have diabetes and a portion of your visit with a doctor was in regards to treating your diabetes. Since you haven’t had a claim approved for diabetes, it’s not an accepted illness and the DOL won’t pay for any treatment related to diabetes.
There are ways to add additional or consequential diagnoses and expand your benefits coverage. We’ll discuss these later on in this post.
The EEOICPA White Medical Card
For living workers, they will be issued a “white benefits card.” This card acts like an insurance card and can be presented to medical providers as payment.
On the front of the card are listed ICD-9 medical codes which correspond to your accepted illnesses. They let medical providers know which services they can bill the DOL for on your behalf.
As you will see pictured below, the card can have many codes listed on it.
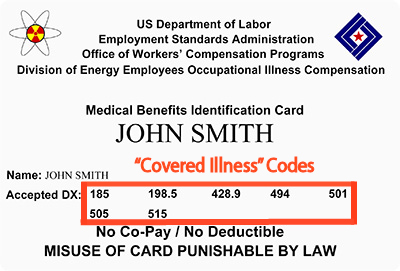
To look up ICD-9 codes and see corresponding medical conditions you can use this government database.
If you search the code 505 you’ll see it corresponds to a Pneumoconiosis diagnosis, which is an occupational lung disease. This means a health provider can bill the DOL for any service related to Pneumoconiosis, such as oxygen or breathing treatment.
What is a Consequential Illness?
Many workers don’t realize that medical conditions or complications as a result of an accepted diagnosis can be added to their medical card. These conditions are considered a consequence of your accepted illness and can therefore be covered.
Per the Department of Labor’s Manual…
“Any illness, injury, impairment, or disease shown by medical evidence to be a consequence of an accepted Part B or Part E condition is covered for medical benefits under the Act. Additionally, under Part E, any illness, injury, impairment, or disease shown by medical evidence to be a consequence of a covered Part E condition may affect the calculation of an impairment rating and/or wage-loss.”
Consequential conditions can greatly expand medical coverage and help workers get the care they need. There are actually 4 different ways for a condition to be considered consequential.
4 Types of Consequential Illness
- Metastasized Cancer – any secondary cancer that originates from the primary cancer site
- Conditions resulting from medical treatment of the accepted illness – such as cataracts caused by chemotherapy
- Natural progression and/or development – such as beryllium sensitivity developing into chronic beryllium disease
- Independent incidents related to an accepted condition – such as a traffic accident injury while traveling for treatment of an accepted condition
Psychological conditions resulting from treatment can also sometimes be added as a consequential illness. The Department of Labor explicitly states; however, psychological conditions must be linked to the accepted condition by the attending physician and a Board-certified psychologist.
To add a consequential illness to your medical card you’ll need to file a new claim with the Department of Labor.
The DOL provides more information on consequential illnesses in the EEOICPA procedure manual
Past Medical Expenses?
The Department of Labor will cover past medical expenses from the date a claim was filed.
For example, if you submitted your claim on January 1st, 2014 but the claim wasn’t approved till January 1st, 2015, all your medical bills associated with the claim would be reimbursed from January 1st, 2014 onward.
Any medical bill prior to January 1st, 2014 would not be eligible for reimbursement since it was before your claim was filed.
It’s important to note that you will need to pay out of pocket or by other means while you wait for a claim to be approved.
Survivors can also seek reimbursement for medical bills incurred once a claim was filed. In the unfortunate event a worker dies while waiting for approval, medical costs can still be recovered by the surviving family.
Time Limits for Reimbursement
Some medical costs, such as travel costs, do have time limits for when bills need to be submitted for reimbursement. Make sure to speak with your local resource center for information on time sensitive reimbursements.
Ongoing services such as home health care, are reevaluated and approved every 6 months based on the patients condition.
Have you submitted a claim yet? Learn more about eligibility under the Energy Employees Occupational Illness Compensation Program.
Let’s Get Started
Filling out the info below will allow us to begin determining your eligibility. Learn more about EEOICPA eligibility.

